



What do members actually want from a health plan experience?

American health insurance has two major problems: member experience and rising care costs. Member experience can suffer when health plans aren’t sure what their members want or expect. However, Wellframe’s recent survey highlights some surprising trends in how members think about their health plans.
To give health plans a clearer picture of what members want, Wellframe commissioned a survey. More than 1,000 people across the U.S. with public or private health insurance responded.
Despite roadblocks and frustrations, many American consumers believe health plans are beneficial overall. Respondents believed health plans want to improve their health proactively, solve health issues quickly, and make life easier—providing a crucial opportunity for health plans to serve as the unlikely heroes of member advocacy.
2021 Health Plan Member Engagement Survey Results
Many survey respondents indicated they would utilize support services offered by health plans:
Navigating the healthcare system
Digital Advocacy
Personalized Care


A care advocate can help direct members to the right providers for their unique needs, and can help secure a referral


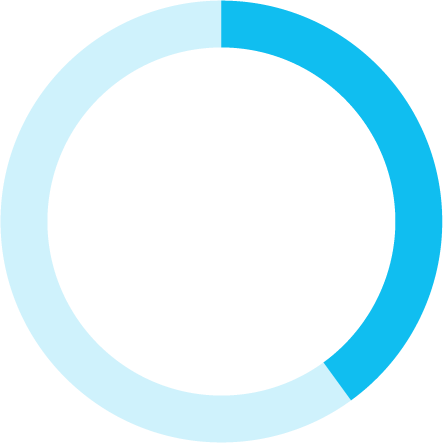
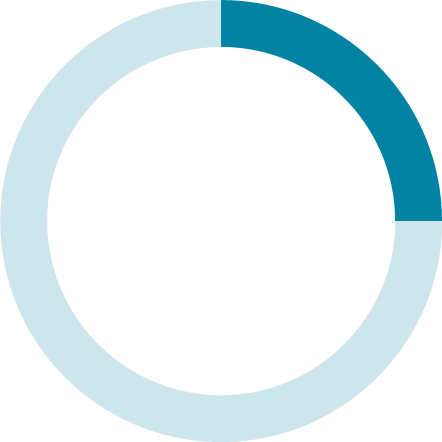
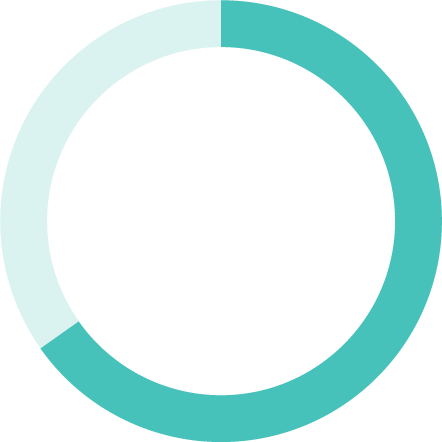
Said they would use a service that could help find and schedule an appointment with a doctor who would be best for specific health needs
Up from 80% in 2020


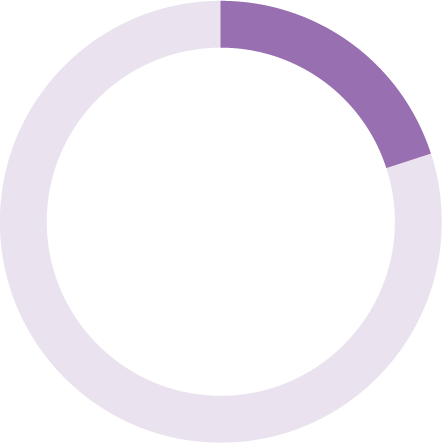
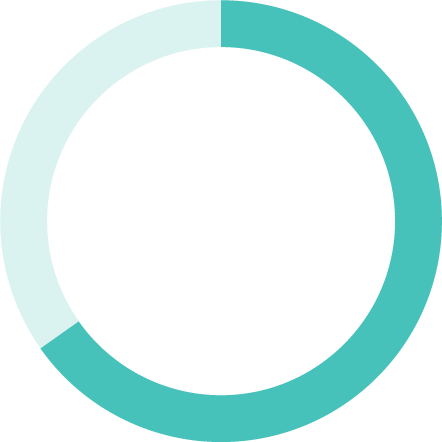
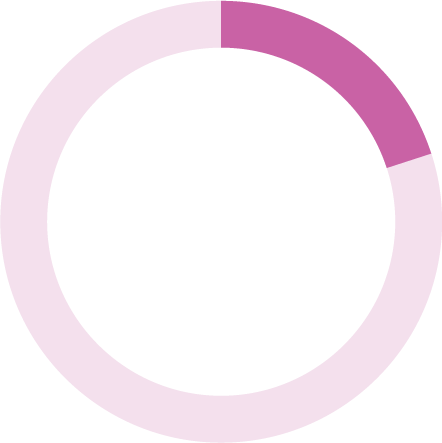
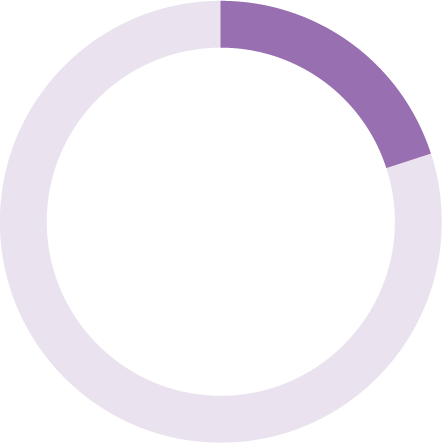
Said information and care they receive is too generic or not personalized.


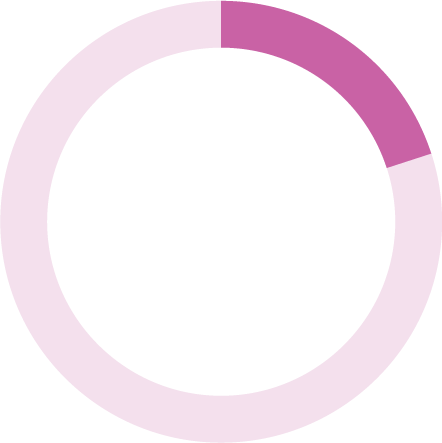
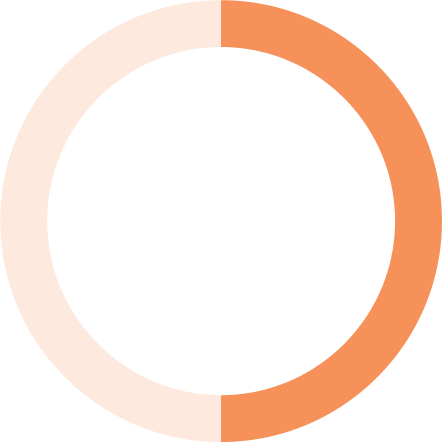
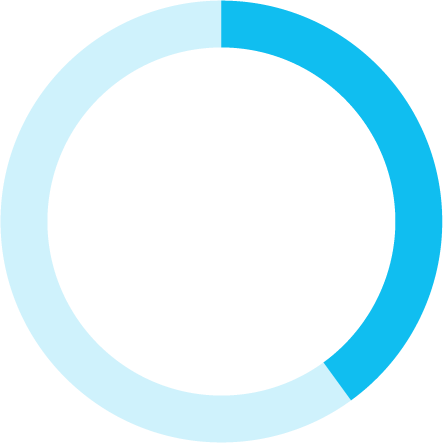
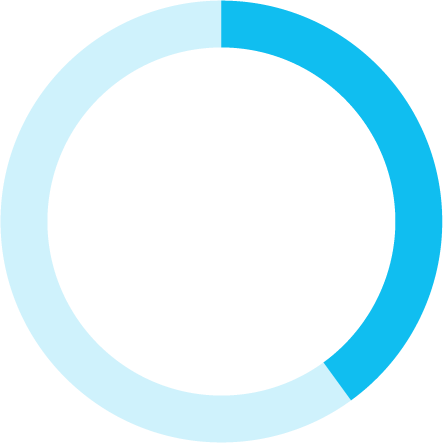
Said they disengaged from their healthcare when they didn’t have the availability to meet with a healthcare provider


Don’t think their healthcare insurance provider understands them and cares for their well-being


43%
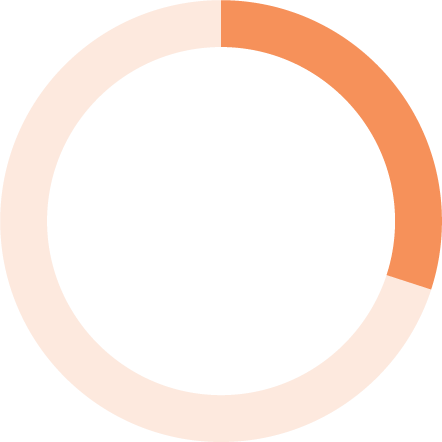
Said they don’t understand their health insurance coverage and benefits.


19%
21%
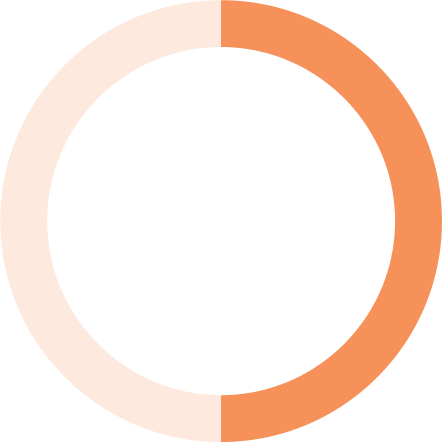
49%
Down from 60% in 2020
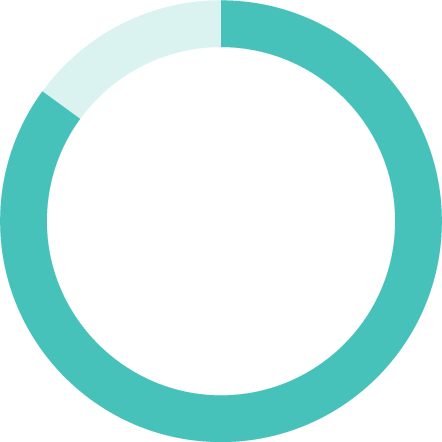
85%

Members want more from their health plans—more personalization and more partnership.
The health plan experience suffers when members become too overwhelmed to self-serve and can’t reach the right staff members for answers. Digital advocacy solutions can help care teams explain benefits and send informational articles to more members than traditional phone outreach.
Compared to 2020, more members are receiving the personalized care they expect. And they’re willing to work with their care teams to access the right care.
Features like secure chat services allow for more consistent communication between care managers and members, promoting greater trust and more beneficial working relationships.
The study revealed that many individuals with chronic conditions are struggling to manage their health during the pandemic. Digital tools can help.
These members need additional support to better manage their own health between doctor visits. Care managers can use features like secure messaging and daily checklists to help keep members on track with their care plans, keeping them healthier and reducing the odds of readmission.
Supporting members with chronic conditions
50%
Condition monitoring, like taking a blood sugar measurement
56%
Medication reminders
65%
An explanation of benefits and eligibility
68%
Finding a care provider and appointment scheduling
Of those surveyed, 64% experience a chronic condition, with most common conditions being mood disorders, arthritis, asthma and diabetes.
One-third (35%) say they only proactively manage their health between doctor’s visits “somewhat well” or “not well."
64%
16%
17%
12%
12%
mood
disorders
arthritis
asthma
diabetes
45% of those with a chronic condition sought support from their health plan for mental health concerns during the pandemic.
One-third of respondents (35%) say they only proactively manage their health between doctor’s visits “somewhat well” or “not well.”








10%
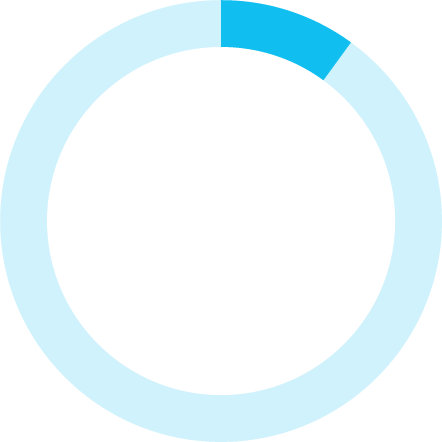
Skip a step in their care plan daily.
20% skip a step weekly.
24%
Missed one or more appointments with a healthcare provider
26%
Forgot to take a dose of their prescription
47%
Would feel most inspired to take action on their health and well-being virtually (through a mobile app, by phone, via web, or via video)
Mental health barriers and reaching vulnerable members
Mental health
Vulnerable members
Social determinants of health, such as household income, can make it more difficult for individuals to manage their health and access care. But care management technologies can bridge the communication gap through two-way chat functions members can use and respond to at their convenience.


Didn’t have the availability to meet with a healthcare provider


22%
Had difficulty finding a healthcare provider and/or making appointments


31%
Have an annual household income below $20k
Physical health is deeply intertwined with mental health, and the pandemic has only exacerbated this issue for individuals with chronic conditions. However, holistic digital health tools may be the solution members need to manage their well-being.


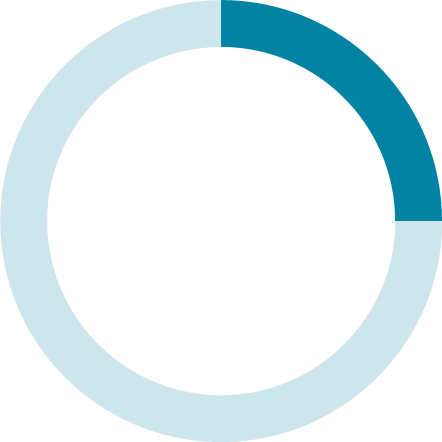
65%
Of members with mood disorders (depression, anxiety, etc.) sought mental health support from their health plan


38%
Have sought support from their health plan for mental health concerns since the start of the pandemic in March 2020


21%

Despite misconceptions, older Americans are interested in leveraging digital health technologies—and many are already using it. In fact, the median age of Wellframe users is 54, with nearly half of members being over 50.
Seniors and healthcare technology

43%
Digital health coaching, such as encouragement for nutrition and exercise
78% would use a service to help them find and schedule an appointment with a doctor who would be best for their specific healthcare needs
One-third of seniors say virtual care would most inspire them to take action on their health and well-being



The U.S. healthcare system has a ways to go before it is accessible to everyone. But we did notice several positive trends among survey respondents. Health plans are still in the right place to be healthcare’s unlikely heroes.
Bright spots
42% said they’d been frustrated when seeking help from their health plan.
However, most people believe insurance wants to:
42%
improve their
health proactively
solve health issues quickly
make life easier
60%
58%
52%
Health plans play a key role in supporting members and improving their experiences. Their leadership teams can coordinate with providers to ensure members have access to the information they need to make informed health decisions and make the most of their benefits.
Making the shift from sporadic outreach to a continuous journey can make all the difference for members living with multimorbidities. Health plans have the power to coordinate care teams and resources to maximize member reach and improve care outcomes.
Takeaway


52%
47%
Female
32%
18–34
years old
32%
35–55
years old
36%
55+
years old
Male
Wellframe worked with a third-party provider to collect responses from over 1000 U.S. adults with public or private insurance.
About this survey
Other
22%
Blue Cross Blue Shield
22%
United
Healthcare Group
14%
Aetna
8%
Anthem
5%
Cigna
4%
Wellcare
3%
Health Care Service Corp.
2%
MCNA Insurance
0.04%
Molina Healthcare
2%
Kaiser Permanente
5%
Humana
6%
0.62%
Non-binary
0.53%
Did not answer








61%
White
17%
Hispanic
14%
Black or
African-American
5%
Asian
1%
American Indian or Alaska Native
0.6%
Native Hawaiian or other Pacific Islander
1%
Did not answer
Are your members falling behind?
How can you engage senior members?
Seniors would use a virtual health tool that offered:
Plan breakdown:
Race breakdown:
Gender breakdown:
Age breakdown:


Interacting with members in more continuous and personalized ways keep them more engaged in their health and with their care teams. By leveraging digital health management, health plans are ideally equipped to close gaps in care and help their members live healthier, happier lives.
Deliver the seamless digital experience members demand.
Request a DEMO today
Health plans have the experience and resources to own their member relationships.
45%
26%
Without a chronic condition
With a chronic condition

64%
mood
disorders
16%
asthma
12%
diabetes
12%